These models are categorized into various types, each providing valuable insights into different aspects of cancer behavior and treatment responses. Researchers use tumor models to study how tumors grow, interact with surrounding tissues, metastasize, and how they respond to targeted therapies, immunotherapies, and chemotherapies. Below is an exploration of the primary types of tumor models and their applications in research.
1. In Vitro Tumor Models
In vitro models involve growing cancer cells outside a living organism, typically in petri dishes or flasks. These models are the foundation of early-stage cancer research, allowing scientists to test drugs, study cellular responses to various stimuli, and understand molecular pathways involved in cancer development.
Monolayer Cultures: This is the most traditional form of in vitro culture where cells grow in a flat, 2D layer. Though commonly used, these cultures fail to replicate the complexity of in vivo tumors, particularly their three-dimensional architecture and interactions with surrounding tissue.
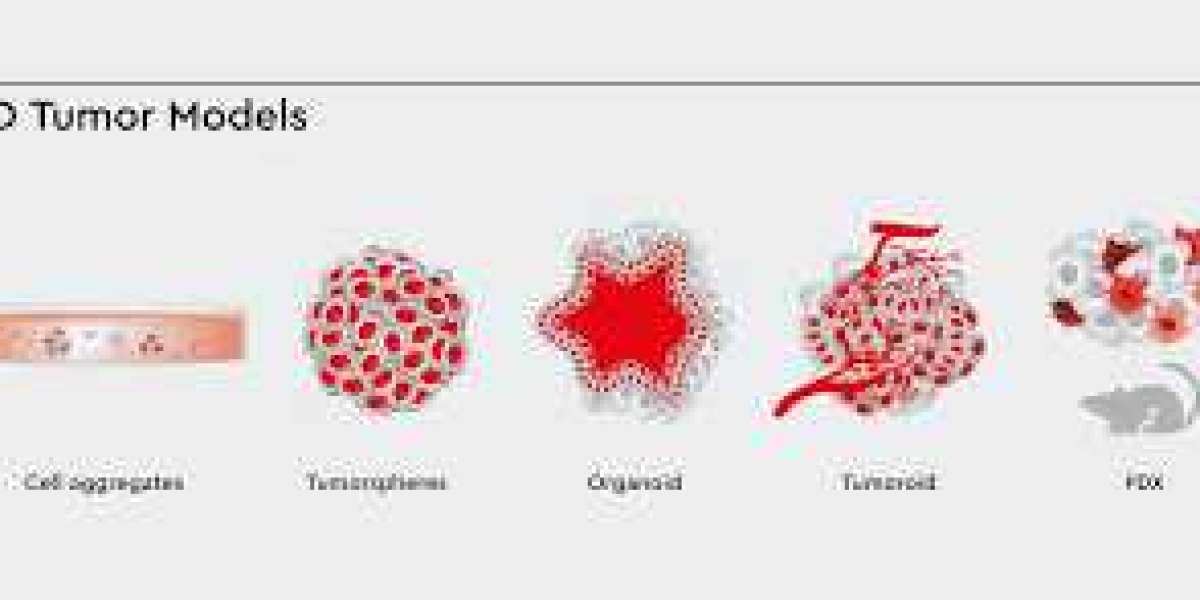
3D Cultures: More advanced than 2D monolayers, 3D cultures enable cells to form spheroids or organoids, mimicking the tumor's natural structure. These models are used to study the impact of the tumor microenvironment, nutrient diffusion, and drug resistance mechanisms more effectively.
Advantages: In vitro models are easy to manipulate and cost-effective, allowing high-throughput screening of potential therapies.
Limitations: These models do not mimic the full complexity of the in vivo tumor environment, such as interactions with immune cells, blood vessels, or distant organs.
2. In Vivo Tumor Models
In vivo models involve implanting tumor cells or tissues into living organisms (often rodents) to observe cancer behavior in a more natural biological context. These models are used to study tumor growth, metastasis, and responses to therapies in a living system, which includes interactions with the immune system, blood vessels, and other tissue types.
a) Syngeneic Models
Syngeneic tumor models involve implanting cancer cells from one animal into another of the same genetic background. This allows the immune system of the host to recognize and interact with the tumor, making these models valuable for immunotherapy research.
- Applications: Studying immune system interactions with tumors and testing immune-modulating therapies like checkpoint inhibitors.
- Advantages: These models allow the immune system to respond to tumors in a natural way, providing more relevant insights into immunotherapy.
- Limitations: They are species-specific, limiting their use to a narrower range of tumor types.
b) Xenograft Models
Xenograft models are created by implanting human tumor cells into immunocompromised animals (often mice). These models are used to study human cancer biology in vivo, as the implanted human tumors retain much of their original biological characteristics.
- Applications: Testing human-specific therapies, including chemotherapy, immunotherapies, and targeted treatments.
- Advantages: These models closely replicate human tumors, making them useful for preclinical testing.
- Limitations: The absence of a functioning immune system in the host animal means these models cannot accurately study immune responses to cancer therapies.
c) Patient-Derived Xenografts (PDX)
PDX models are developed by implanting tumor tissue directly taken from a patient into an immunocompromised mouse. These models closely mirror the genetic and histological features of the patient’s original tumor, providing valuable insights into personalized medicine.
- Applications: PDX models are used for testing individualized drug treatments, evaluating the effectiveness of therapies in a patient-specific context.
- Advantages: They retain the heterogeneity and complexity of human tumors, making them ideal for personalized cancer research.
- Limitations: PDX models are time-consuming to establish and expensive to maintain.
d) Genetically Engineered Mouse Models (GEMMs)
GEMMs are mice that have been genetically modified to develop cancer, either through the insertion of oncogenes or the deletion of tumor-suppressor genes. These models are designed to mimic the genetic mutations found in human cancers.
- Applications: Studying the genetic basis of cancer, investigating specific mutations, and exploring how genetic changes lead to tumor initiation and progression.
- Advantages: GEMMs allow researchers to study the effects of specific genes and mutations in the context of the whole organism.
- Limitations: These models are complex and can take a long time to develop, which makes them costly and resource-intensive.
3. Tumor Organoid Models
Organoids are 3D structures derived from patient tissue or stem cells that replicate the cellular complexity of a tumor. These models can be grown in the lab to study cancer biology and therapeutic responses.
- Applications: Tumor organoids can be used to evaluate drug efficacy, study tumor biology, and model the tumor microenvironment.
- Advantages: These models are more physiologically relevant than traditional cell culture models and can provide insights into how tumors respond to treatments.
- Limitations: Although they mimic many aspects of human tumors, organoid models still lack the complete tumor microenvironment, including immune cells and blood vessels.
4. Tumor Microenvironment Models
The tumor microenvironment (TME) plays a critical role in cancer progression and therapy resistance. Models of the TME are used to study how the surrounding tissue, immune cells, and blood vessels interact with the tumor, and how these interactions influence tumor growth and metastasis.
- Applications: Tumor microenvironment models are used to study immune evasion, angiogenesis (the formation of new blood vessels), and the response of tumors to therapies.
- Advantages: These models help to understand the complex interactions that occur in the tumor environment.
- Limitations: Recreating the full complexity of the TME in vitro or in vivo remains challenging.
Applications of Tumor Models in Cancer Research
Drug Discovery and Development: Tumor models play a crucial role in identifying potential drug candidates and testing their efficacy in preclinical stages. They allow researchers to screen large numbers of compounds for anti-cancer activity.
Cancer Immunotherapy: Animal tumor models are instrumental in studying the effectiveness of immunotherapies, such as checkpoint inhibitors, CAR-T cells, and cancer vaccines, by simulating immune system interactions with tumors.
Tumor Metastasis: Animal models, particularly orthotopic and GEMMs, allow for the study of how cancer spreads to other organs, providing valuable insights into metastasis and helping researchers develop therapies aimed at preventing or treating metastatic cancer.
Personalized Medicine: Tumor models like PDX and organoids are invaluable in the development of personalized treatments. By using models derived from patients’ own tumors, researchers can test a variety of drugs to determine the most effective treatment for that specific patient.
Challenges and Future Directions
Species Differences: Animal tumor models often fail to completely replicate human cancer, especially in terms of tumor progression and drug responses. The differences between species can limit the applicability of results to human patients.
Immune System Limitations: Many models, especially xenografts, involve immunocompromised animals, which can limit the ability to study immune-related therapies accurately.
Ethical Considerations: The use of animals in cancer research is a subject of ongoing ethical debate, and there is a growing emphasis on reducing animal use, refining animal models, and finding alternative methods, such as organoid models, to study cancer.
Model Complexity: Developing more sophisticated models that better mimic human tumors, including the immune system and microenvironment, is an ongoing challenge. Future research will likely focus on overcoming these limitations and creating more accurate models.
Conclusion
Tumor models are fundamental tools in cancer research, helping scientists understand the complex biology of cancer and test new therapeutic approaches. Although there are limitations in current models, advances in technology, such as patient-derived models, organoids, and genetic engineering, continue to improve the relevance and accuracy of these models. The ongoing development of more human-like tumor models will play a crucial role in advancing cancer treatment and providing more effective therapies for patients.